Edmonton Concussion Treatment
Traumatic brain injuries often have multiple trajectories. Usually, rehabilitation often has the best outcome with a multi-disciplinary approach. Dependent upon each patient’s particular symptoms and diagnoses, the appropriate treatment may vary.
Disciplines participating in the rehabilitation of traumatic brain injury should include optometrists, physiotherapists, physicians, occupational therapists, psychologists, speech pathologists, and chiropractors. Other professions may be required depending on the patient’s specific symptoms.
What is Traumatic Brain Injury?
Traumatic brain injury (TBI), such as a concussion, occurs when the brain experiences sudden or severe damage. Caused by an external force, types of injuries can include motor vehicle accidents, falls, and sports injuries. Injuries range from mild to severe permanent brain damage. Most concussions fall within the mild category which are often very responsive to vision therapy rehabilitation if visual issues occur.
Symptoms of a concussion – What you may be told by an injured person:
- Headache or “Pressure in the head”
- Dizziness or balance problems
- Mental clouding, confusion, or feeling slowed down
- Trouble seeing
- Nausea or vomiting
- Fatigue
- Difficulty concentrating
- Sensitivity to light or noise
- Difficulty with reading, learning or work
- Sleep problems: falling asleep / too much or too little
- Emotional / anger / sad / anxious
Edmonton Vision Therapy for a Traumatic Brain Injury
Patients who have experienced concussions, stroke, or have been in a motor vehicle accident can benefit from concussion treatment to address a variety of visual symptoms. These symptoms may include light sensitivity, balance issues, dizziness, double vision and/or visual memory problems.
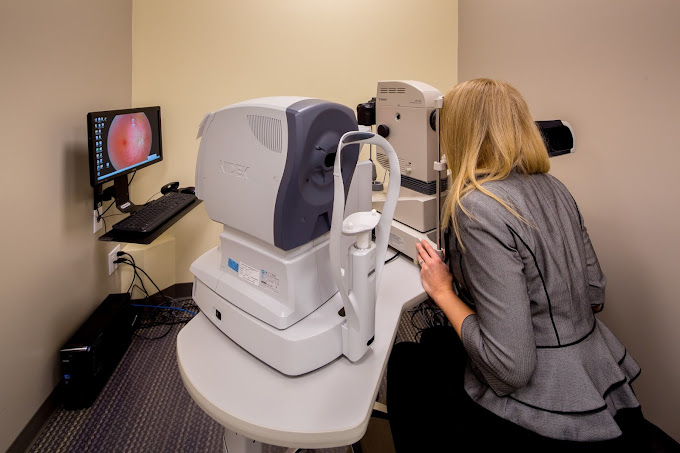
The vision issues that result from concussions can affect your ability to visually judge where objects are located in space, or where your body is positioned in space. This can impact balance and coordination, which is especially concerning for those returning to sports, training, or daily activities. Eye movements are often affected causing difficulty reading, or blurry and fluctuating vision. Oftentimes, concussion patients still see 20/20, so these issues may not show up on a routine eye exam without additional testing.
Recovery from post-concussion vision issues may involve specialized glasses. These may contain tint, prism, occlusion, or modified lens designs to help the brain process visual information more efficiently. Glasses can also improve reading performance, coordination, and balance issues, aiding in overall recovery.
Vision therapy is an effective part of recovery for individuals with traumatic brain injuries. Committed to providing therapy services at our Edmonton-based clinic, Vision by Design offers personalized concussion treatment. Our program is under the direct supervision of Dr. Sarah Keep or one of our qualified optometrists. Our patients receive high-quality care tailored to their needs, so if you are in Edmonton and experiencing visual symptoms, book an appointment to start your recovery journey today.
Side Effects of a TBI
Our vision is highly dependent on our brain. Half of our brain pathways relate to visual function. As a result, patients suffering with TBI can experience:
Eye Tracking
Eye movements, or ocular motor skills, are important for our eyes to be able to gather visual information. We have to be able to maintain a steady gaze on a target, follow a moving object, or shift our eyes from one target to another. Activities like reading and driving greatly depend on these skills. When a patient has suffered a concussion or other traumatic brain injury, these skills can be greatly affected. Patients experiencing difficulties with these ocular motor skills may lose their place when they read, skip words or lines, or read words out of order. Deficiency in these skills can also affect coordination in sports or for activities such as driving. Some patients can experience nystagmus, an ocular condition that affects visual clarity and balance as the eyes continually move on and off their intended target.
Eye Focusing
Our eyes have to be able to change focus from one distance to another to create a clear image. Patients with traumatic brain injuries often lose the ability and endurance to switch focus between objects at various distances. The resulting symptoms include fluctuating blurry vision, headaches, eye strain, and difficulty performing near work for extended periods.
Visual Perceptual Skills
TBI patients often have difficulty with visual perceptual processing. Visual perceptual skills allow us to make sense of the visual information received by the brain. Difficulty with visual perceptual processing can result in a TBI patient experiencing a cognitive “fog”. This “fog” affects several aspects of vision including:
- Visual attention span
- Visual processing speed
- Visuospatial memory
- Visual memory
- Light & Visual Sensitivity
Light & Visual Sensitivity
It is quite common for patients with TBI to develop a hypersensitive visual system. Sensitivity to light and other changes to the visual environment can be especially challenging. The ability to filter out visual noise is impaired, which can make large crowds and visual motion especially overwhelming for TBI patients because they are unable to ignore irrelevant visual input. Additionally, patients can experience balance issues as they are unable to rely on the visual input that allows us to recognize our body’s position in space.
Visual Hallucination
TBI sufferers can experience visual hallucinations that appear as stars, flashes or spots, as well as perceived motion of objects. These hallucinations may occur when the brain misunderstands visual information due to damage to the brain tissue. This results in disruptions to how the brain processes information.
Eye Teaming
The ability of the eyes to coordinate is commonly affected by a traumatic brain injury. Effective eye-teaming occurs when both of our eyes have to move in a coordinated manner to ensure they are pointing at the same target. The inward movement of our eyes to aim at a near target is called convergence and the outward movement to aim our eyes at a distant target is called divergence. Accurate eye teaming is often lost following a traumatic brain injury such as a concussion. Patients with reduced convergence or divergence may experience double vision, eye strain, words moving on a page and/or reduced depth perception.
Visual Field Loss
It is possible for a patient with a traumatic brain injury to have a hemianopsia or a visual field defect. When this occurs, a patient will either have the vertical half, or horizontal half of their vision missing. Patients who have visual field loss often have difficulty with certain daily activities or may be at risk for a fall or injury. Certain accommodations can be taught to patients to help them better perform activities with a field defect. It can also be possible to see some improvement in the visual field by performing certain scanning activities.

Concussion Treatment FAQs
What is the prognosis for recovery after concussion treatment?
The prognosis for most mild traumatic brain injuries, such as a concussion, depends on how long symptoms are present. A well-structured treatment plan plays a crucial role in concussion recovery and can improve outcomes.
If symptoms persist for longer than three months past the initial injury, the prognosis tends to be worse or may require additional concussion rehab to support symptom management and recovery.
Other individual factors can also affect prognosis, such as the number of previous head injuries, a history of anxiety or depression, the severity of injury, prior neurological disease, persistent physical illness, or advanced age. Working with a specialized health care team can help address these factors and improve recovery outcomes.
How does neuro-optometric vision therapy work services help concussion recovery?
A traumatic brain injury can lead to damaged pathways in the brain. This disruption can interfere with communication between different areas, making concussion management more complex.
This prevents our brain from using these damaged connections to process visual information. A targeted treatment plan through neuro-optometric rehabilitation can help train the brain to rewire its connections and use other areas to compensate for damage.
This results in better communication throughout the brain, improving symptoms and enhancing concussion rehab efforts. A collaborative, multi-disciplinary approach ensures a well-rounded recovery strategy.
How long until I see results?
Each case presents varying degrees of symptoms. However, studies show that most patients can anticipate at least 6-10 weeks of visual rehabilitation before noticeable improvements occur.
Active participation in a structured concussion recovery program, including therapy and monitored activity, can help accelerate progress. It is common to require additional weeks to embed the new skills so that regression does not occur once rehabilitation is complete. Consistently following a personalized treatment plan is key to long-term success.